When it comes to brain tumors, astrocytoma is one of the most frequently encountered types. Although the term may sound intimidating, understanding what astrocytoma is, how it develops, and the treatment options available can help patients and families feel more prepared and hopeful.
In this blog, we’ll explore astrocytoma in depth — from its origins to symptoms, diagnosis, and treatment.
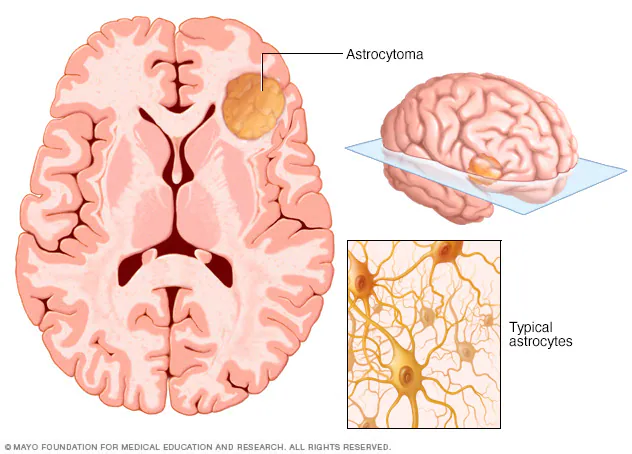
Astrocytoma is a type of tumor that develops from astrocytes, star-shaped cells that are part of the brain’s supportive tissue. Astrocytes play a key role in maintaining the health of neurons, providing them with nutrients, and repairing the brain and spinal cord after injury.
Astrocytomas belong to a larger group of tumors called gliomas, which are tumors that arise from glial cells. Astrocytomas can occur in the brain or spinal cord and vary widely in their behavior — some are slow-growing and benign, while others are aggressive and malignant.
Types and Grades of Astrocytoma
Astrocytomas are classified by the World Health Organization (WHO) into different grades based on how the tumor cells look under a microscope and how quickly they are likely to grow:
- Grade I (Pilocytic Astrocytoma): A slow-growing, often noncancerous tumor usually found in children and young adults. It can often be cured with surgery.
- Grade II (Diffuse Astrocytoma): A slow-growing tumor but one that can infiltrate nearby brain tissue, making complete removal challenging.
- Grade III (Anaplastic Astrocytoma): A faster-growing and more aggressive tumor that typically requires more intensive treatment.
- Grade IV (Glioblastoma): The most aggressive form, also known as glioblastoma multiforme (GBM), characterized by rapid growth and spread within the brain.
Understanding the grade of an astrocytoma is crucial because it heavily influences treatment decisions and prognosis.
Causes and Risk Factors
The exact causes of astrocytomas are not fully understood. However, certain risk factors are known to contribute:
- Genetic mutations: Changes in specific genes, such as TP53 and IDH1, are often found in astrocytoma cells.
- Radiation exposure: Previous radiation therapy to the head, especially during childhood, can increase the risk of developing brain tumors.
- Family history: Although rare, some inherited syndromes, like Li-Fraumeni syndrome or neurofibromatosis type 1, are associated with a higher risk of gliomas.
Most astrocytomas, however, develop sporadically without any identifiable risk factors.
Symptoms of Astrocytoma
The symptoms of astrocytoma depend on the tumor’s size, location, and growth rate. Common signs and symptoms include:
- Headaches: Often worse in the morning or when lying down.
- Seizures: A frequent early symptom, especially in low-grade astrocytomas.
- Cognitive or personality changes: Difficulty thinking, memory loss, mood swings, or depression.
- Nausea and vomiting: Related to increased pressure inside the skull.
- Weakness or numbness: Particularly if the tumor affects areas controlling movement or sensation.
- Vision or speech problems: If tumors are near vision-processing or language areas of the brain.
Because these symptoms can be subtle and progress slowly, it’s important to seek medical evaluation for persistent neurological symptoms.
How is Astrocytoma Diagnosed?
Diagnosing astrocytoma involves a series of steps:
- Neurological examination: To check for signs of brain dysfunction.
- Imaging tests: MRI scans are the most effective method for detecting brain tumors. CT scans may also be used in some cases.
- Biopsy: A sample of tumor tissue is taken either during surgery or via a needle biopsy. It is then analyzed to determine the type and grade of the tumor.
- Molecular testing: Identifying genetic mutations can help in tailoring personalized treatments.
Early and accurate diagnosis is critical for creating an effective treatment plan.
Treatment Options for Astrocytoma
The approach to treating astrocytoma varies based on the tumor’s grade, size, and location, as well as the patient’s age and overall health.
Surgery
- Whenever possible, the goal is to surgically remove as much of the tumor as safely possible.
- In low-grade astrocytomas, complete removal can sometimes be curative.
Radiation Therapy
- Often used after surgery, especially if some tumor tissue remains or if the astrocytoma is high-grade.
- Can also be the primary treatment if surgery is not possible.
Chemotherapy
- Drugs like temozolomide are commonly used to treat higher-grade astrocytomas, often in combination with radiation therapy.
- Chemotherapy can help control tumor growth and extend survival.
Targeted Therapy and Clinical Trials
- Newer treatments targeting specific genetic mutations are under study.
- Clinical trials may offer additional options for some patients.
Supportive Care
- Medications to control seizures, reduce brain swelling, and manage other symptoms play a crucial role in improving quality of life.
Living with Astrocytoma
A diagnosis of astrocytoma can be life-changing, but many people live meaningful lives after treatment. Regular follow-up scans, rehabilitation therapy, and support services are important parts of ongoing care.
Emotional support, whether from family, support groups, or counseling, can make a significant difference in coping with the challenges of living with a brain tumor.
Conclusion
Astrocytoma is a diverse group of brain tumors that can range from slow-growing and manageable to aggressive and life-threatening. Advances in imaging, surgical techniques, and targeted therapies have greatly improved outcomes for many patients. Early diagnosis, individualized treatment, and a strong support system are vital for navigating the journey with astrocytoma.
The list of some Astrocytoma medicine:
Lucivora