Filariasis is a parasitic disease that has silently affected millions across the globe, particularly in tropical and subtropical regions. Despite its widespread impact, many people are unfamiliar with the condition until it personally affects them or their communities. By understanding what filariasis is, how it spreads, and how it can be treated and prevented, we can take steps to combat this neglected tropical disease.
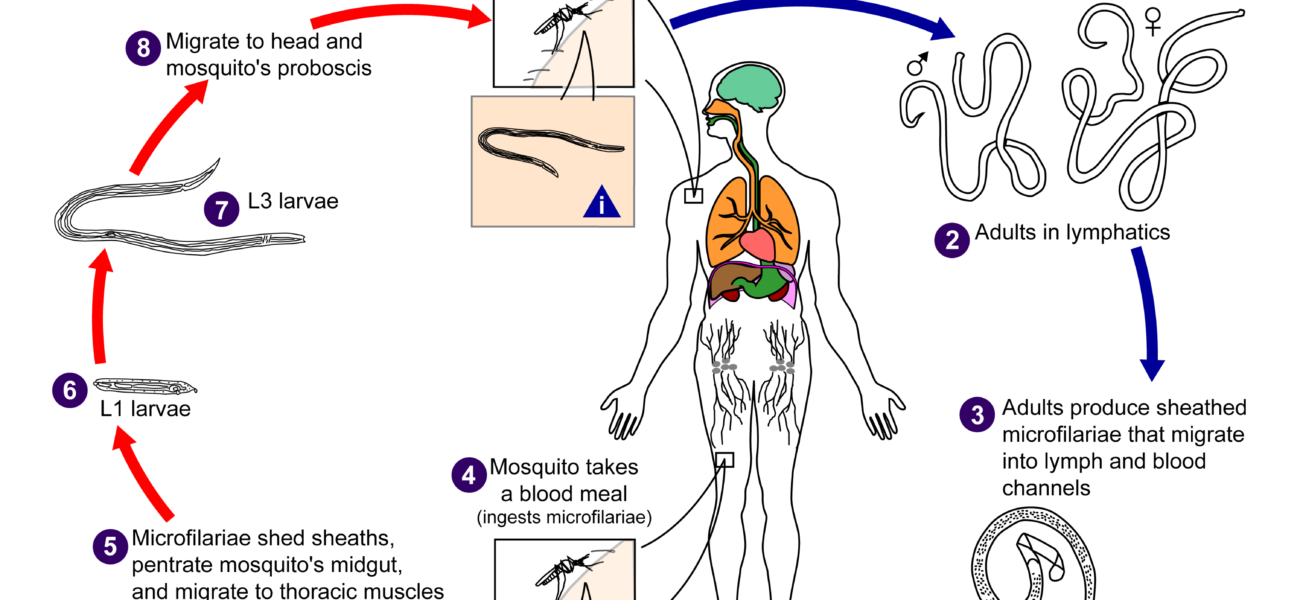
Filariasis is caused by infection with filarial worms, tiny thread-like parasites transmitted to humans through the bites of infected mosquitoes. Once inside the body, these parasites travel to the lymphatic system, which is responsible for maintaining fluid balance and fighting infections.
There are several types of filarial worms, but the most common form of the disease is lymphatic filariasis, caused by species like Wuchereria bancrofti, Brugia malayi, and Brugia timori. Over time, the infection can cause severe damage to the lymphatic system, leading to a range of physical symptoms and long-term disability.
How is Filariasis Transmitted?
The primary mode of transmission for filariasis is through mosquito bites. When a mosquito feeds on the blood of an infected person, it ingests microscopic larvae called microfilariae. These larvae develop inside the mosquito and are later transferred to another human when the mosquito feeds again.
Filariasis is typically found in areas with:
- Poor sanitation
- Stagnant water sources
- Dense mosquito populations
The disease often thrives in poverty-stricken regions, making it not only a health issue but also a social and economic concern.
Symptoms of Filariasis
In the early stages, filariasis infections may not cause any noticeable symptoms, allowing the parasites to quietly damage the lymphatic system. However, as the infection progresses, the following symptoms may appear:
- Swelling (Lymphedema): Usually in the legs, arms, breasts, or genital areas.
- Elephantiasis: Thickening and hardening of the skin and underlying tissues, leading to severe disability.
- Fever and chills: Often associated with inflammation of the lymph nodes.
- Pain: In swollen or inflamed areas.
Chronic filariasis can cause emotional distress, social stigma, and economic hardship due to reduced mobility and work capacity.
Diagnosing Filariasis
Diagnosis typically involves:
- Blood tests: Microfilariae are often detectable in blood samples taken at night, when the parasites are most active in the bloodstream.
- Ultrasound: May reveal adult worms in the lymphatic system.
- Antigen tests: Can detect proteins released by adult worms, even when microfilariae are not present in blood samples.
Early diagnosis is crucial for effective management and prevention of complications.
Treatment Options
Treating filariasis usually involves antiparasitic medications, such as:
- Diethylcarbamazine (DEC): Kills microfilariae and some adult worms.
- Ivermectin: Reduces the number of microfilariae in the blood.
- Albendazole: Often used in combination with DEC or ivermectin.
In cases of advanced disease, additional treatments may be necessary:
- Care for lymphedema through hygiene, exercise, and elevation of affected limbs.
- Surgery in severe cases of elephantiasis or hydrocele (swelling of the scrotum).
Mass drug administration (MDA) programs, where entire at-risk populations are treated annually, have been crucial in reducing the burden of filariasis globally.
Prevention of Filariasis
Preventing filariasis centers around mosquito control and personal protection:
- Use insecticide-treated mosquito nets while sleeping.
- Wear long-sleeved clothing and use insect repellent.
- Eliminate standing water where mosquitoes breed.
- Participate in community-wide treatment programs to reduce transmission.
In addition, improving sanitation and public health infrastructure plays a vital role in long-term prevention.
The Global Effort to Eliminate Filariasis
The World Health Organization (WHO) has launched initiatives like the Global Programme to Eliminate Lymphatic Filariasis (GPELF), aiming to stop the transmission of the disease through mass treatment and support for those already affected. Several countries have made tremendous progress and are close to eliminating filariasis as a public health problem.
However, sustained efforts are necessary to prevent resurgence and ensure that communities receive the care and resources they need.
Conclusion Filariasis is a deeply impactful yet preventable disease. By raising awareness, improving mosquito control, participating in treatment programs, and supporting global health initiatives, we can work together to eliminate filariasis and improve the lives of millions. Understanding the disease is the first step toward a world free from its burden.
The list of some Filariasis medicine: