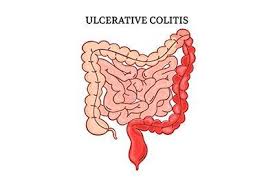
Ulcerative Colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in the lining of the large intestine (colon) and rectum. This condition leads to symptoms such as abdominal pain, diarrhea, rectal bleeding, and fatigue, which can significantly affect daily life.
Unlike temporary digestive issues, ulcerative colitis is a lifelong condition characterized by alternating periods of flare-ups and remission. Understanding its causes, symptoms, and treatment options is essential for proper management and improved quality of life.
What is Ulcerative Colitis?
Ulcerative colitis is an autoimmune-related disorder in which the body’s immune system mistakenly attacks the cells of the colon lining, causing inflammation and ulcer formation. Over time, this inflammation can lead to tissue damage and impaired bowel function.
The disease typically begins in the rectum and may spread upward through parts or the entire colon. It can vary in severity—from mild inflammation to severe, widespread ulceration.
Although the exact cause remains unknown, genetic, environmental, and immune system factors are believed to play a key role in its development.
Causes and Risk Factors
While the precise cause of ulcerative colitis is not fully understood, several contributing factors have been identified:
- Immune system dysfunction: An abnormal immune response attacks healthy intestinal tissue.
- Genetic predisposition: A family history of ulcerative colitis increases susceptibility.
- Environmental factors: Diet, pollution, and certain infections may trigger inflammation.
- Age: Commonly diagnosed between ages 15 and 35, but can occur at any age.
- Ethnicity: More prevalent in people of Caucasian or Ashkenazi Jewish descent.
- Lifestyle influences: Stress, smoking cessation, or high-fat diets can exacerbate symptoms.
Symptoms
Symptoms vary depending on the severity and extent of inflammation but generally include:
- Persistent diarrhea, often with blood or mucus
- Abdominal pain and cramping
- Urgent need to have bowel movements
- Rectal bleeding or pain
- Fatigue and weakness due to blood loss or inflammation
- Unintended weight loss and loss of appetite
- Fever during flare-ups
These symptoms can fluctuate over time, with patients experiencing symptom-free periods (remission) followed by relapses.
Effects on Daily Life
Living with ulcerative colitis can be both physically and emotionally challenging. Frequent bowel movements, dietary restrictions, and fatigue can interfere with work, travel, and social activities.
In addition, the emotional burden—such as anxiety or depression related to flare-ups—can impact mental well-being. With proper medical care, lifestyle adjustments, and emotional support, many people can maintain a fulfilling and active life despite the condition.
Diagnosis
Diagnosing ulcerative colitis requires a combination of medical history review, physical examination, and diagnostic testing to confirm inflammation and rule out other conditions.
Common diagnostic methods include:
- Colonoscopy: The gold standard for visualizing ulcers and taking biopsy samples.
- Blood tests: To detect anemia and signs of inflammation (elevated CRP or ESR).
- Stool tests: Used to exclude infections and measure inflammatory markers.
- Imaging studies: CT or MRI scans may assess the extent and severity of disease.
Accurate diagnosis helps determine the appropriate treatment plan and monitor disease progression effectively.
Treatment Options
The goal of ulcerative colitis treatment is to reduce inflammation, relieve symptoms, and maintain long-term remission. Treatment plans are individualized based on disease severity and response to therapy.
1. Medications
- Aminosalicylates (5-ASA): Such as mesalamine or sulfasalazine to reduce inflammation.
- Corticosteroids: For short-term control of moderate to severe flare-ups.
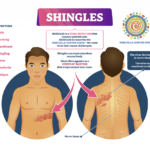
- Immunomodulators: Azathioprine and 6-mercaptopurine help suppress immune overactivity.
- Biologic therapies: Target specific immune pathways (e.g., infliximab, adalimumab, vedolizumab).
- JAK inhibitors: Newer oral treatments like tofacitinib for moderate to severe cases.
2. Surgery
In severe cases unresponsive to medication, surgical removal of the colon (colectomy) may be required. This can provide a permanent cure but requires careful post-surgical management.
3. Dietary and Lifestyle Modifications
- Follow a balanced, low-fiber diet during flare-ups.
- Stay hydrated and avoid caffeine, alcohol, or spicy foods.
- Manage stress through yoga, meditation, or counseling.
- Regular follow-ups with a gastroenterologist to monitor disease activity.
Coping and Lifestyle Management
Adapting to ulcerative colitis involves not only medical care but also emotional and lifestyle adjustments:
- Join support groups to connect with others living with IBD.
- Maintain a food diary to identify trigger foods.
- Incorporate light physical activity to improve overall well-being.
- Prioritize mental health, as chronic illness can affect emotional stability.
- Stay informed about new treatment advances and options.
Final Thoughts
Ulcerative Colitis is a complex yet manageable condition with the right combination of medical treatment, self-care, and support. Advances in medication and biologic therapy have greatly improved symptom control and quality of life for patients. If you or someone you know is experiencing persistent digestive symptoms, early consultation with a gastroenterologist can lead to faster diagnosis and better outcomes.
With consistent care and a proactive approach, living a healthy, balanced life with ulcerative colitis is entirely possible.
The list of some Ulcerative Colitis medicine: