Diabetes is a chronic condition that affects how the body consumes glucose, a form of sugar that serves as the body’s primary source of energy. Diabetes occurs when the body either does not produce enough insulin, a hormone that helps glucose enter the cells, or does not respond properly to insulin. This leads to high levels of glucose in the blood, which can cause various health problems.
According to the Centers for Disease Control and Prevention (CDC), more than 34 million Americans have diabetes, and about 88 million have prediabetes, a condition that increases the risk of developing diabetes. Diabetes is also a major cause of disability and death in the United States and worldwide.
In this blog post, we will explore some of the most common causes, symptoms, and treatment options for diabetes.
Types of Diabetes
There are different types of diabetes, each with its own causes and characteristics. The main types of diabetes are:
• Type 1 diabetes is an autoimmune illness in which the immune system erroneously assaults and kills insulin-producing beta cells in the pancreas. Type 1 diabetes usually develops in childhood or adolescence, but can also occur at any age. People with type 1 diabetes need to take insulin injections or use an insulin pump to control their blood glucose levels.
• Type 2 diabetes: This is the most prevalent kind of diabetes, which happens when the body develops insulin resistance or fails to generate enough insulin. Type 2 diabetes is most common in adults, although it can also occur in children and adolescents. Type 2 diabetes is often associated with obesity, physical inactivity, family history, and genetic factors. People with type 2 diabetes may need to take oral medications or injectable drugs to control their blood glucose levels.
• Gestational diabetes: This is a type of diabetes that occurs during pregnancy when the placenta produces hormones that make the body more resistant to insulin. Gestational diabetes usually goes away after delivery, but it increases the risk of developing type 2 diabetes later in life for both the mother and the child. Women with gestational diabetes need to monitor their blood glucose levels and follow a healthy diet and exercise plan to prevent complications.
• Other types of diabetes: These include rare forms of diabetes that are caused by genetic mutations, diseases of the pancreas or other organs, infections, medications, or other factors. Some examples are monogenic diabetes, cystic fibrosis-related diabetes, drug-induced diabetes, and latent autoimmune diabetes in adults (LADA).
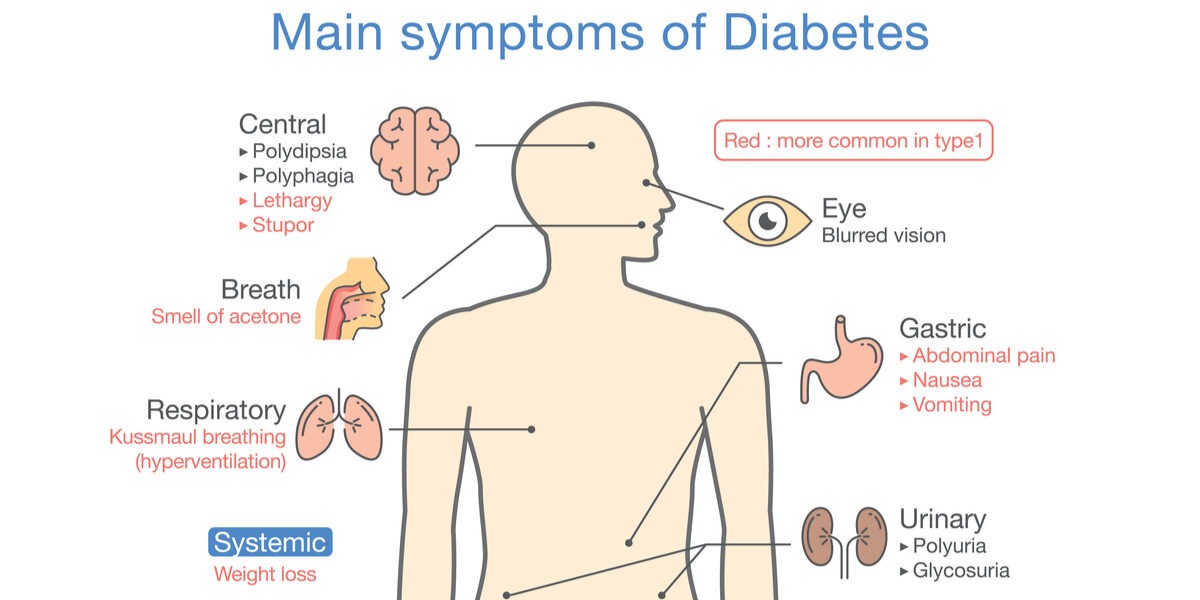
Symptoms of diabetes
The symptoms of diabetes may vary depending on the type and severity of the disease. Some people may not have any symptoms at all or may not notice them until they develop complications. Diabetes symptoms include the following:
• Increased thirst and urination
• Increased hunger
• Unexplained weight loss
• Fatigue
• Blurred vision
• Slow-healing wounds
• Hand or foot numbness or tingling
• Recurrent infections
• Dry skin or itching
Some people with type 1 diabetes may also experience diabetic ketoacidosis (DKA), a life-threatening condition that occurs when there is not enough insulin in the body and the cells start to break down fat for energy. This produces ketones, which are acidic substances that build up in the blood and urine. DKA symptoms include:
• Nausea and vomiting
• Abdominal pain
• Fruity-smelling breath
• Rapid breathing
• Confusion or coma
DKA is a medical emergency that requires immediate treatment with insulin and fluids.
Causes of diabetes
The exact causes of diabetes are not fully understood, but they involve a combination of genetic and environmental factors. Some of the possible causes of different types of diabetes are:
• Type 1 diabetes: The cause of type 1 diabetes is unknown, but it is believed to involve a combination of genetic susceptibility and environmental triggers that activate the immune system to attack the beta cells. Some possible triggers include viruses, bacteria, toxins, chemicals, or dietary factors.
• Type 2 diabetes: The cause of type 2 diabetes is complex and multifactorial, but it involves a combination of genetic predisposition and lifestyle factors that impair insulin action or secretion. Some possible factors include obesity, physical inactivity, poor diet, aging, ethnicity, family history, or hormonal disorders.
• Gestational diabetes: The cause of gestational diabetes is not clear, but it involves a combination of genetic and hormonal factors that make the body more resistant to insulin during pregnancy. Some possible factors include obesity, age, family history, ethnicity, or previous history of gestational diabetes. Diagnosis of diabetes The diagnosis of diabetes is based on blood tests that measure the level of glucose in the blood.
Diabetes is diagnosed using the following tests:
• Fasting plasma glucose (FPG) test: This test measures the level of glucose in the blood after fasting for at least eight hours. FPG levels in the normal range are less than 100 mg/dL (5.6 mmol/L). An FPG level between 100 and 125 mg/dL (5.6 and 6.9 mmol/L) indicates prediabetes. An FPG level of 126 mg/dL (7 mmol/L) or higher on two separate occasions indicates diabetes.
• Oral glucose tolerance test (OGTT): This test measures the level of glucose in the blood before and after drinking a liquid that contains 75 grams of glucose. A normal OGTT result is less than 140 mg/dL (7.8 mmol/L) two hours after drinking the liquid. An OGTT result between 140 and 199 mg/dL (7.8 and 11 mmol/L) indicates prediabetes. An OGTT result of 200 mg/dL (11.1 mmol/L) or higher on two separate occasions indicates diabetes.
• Hemoglobin A1c (HbA1c) test: This test measures the average level of glucose in the blood over the past two to three months by looking at how much glucose is linked to hemoglobin, a protein found in red blood cells. A normal HbA1c level is less than 5.7%. An HbA1c level between 5.7% and 6.4% indicates prediabetes. An HbA1c level of 6.5% or higher on two separate occasions indicates diabetes. Other tests may be used to diagnose other types of diabetes or to screen for complications or risk factors.
Treatment of diabetes
The treatment of diabetes aims to keep blood glucose levels within a normal range and prevent or delay complications. The treatment plan depends on the type and severity of diabetes, as well as individual factors such as age, health status, preferences, and goals.
The main components of diabetes treatment are:
• Medications: These are drugs that help lower blood glucose levels by stimulating insulin production or action, reducing glucose absorption or production, or increasing glucose excretion. The type and dose of medications depend on various factors such as blood glucose levels, kidney function, weight, and side effects. Some common medications for type 1 and type 2 diabetes include:
• Insulin: This is a hormone that helps glucose enter the cells. People with type 1 diabetes need to take insulin injections or use an insulin pump to replace the insulin they do not produce. People with type 2 diabetes may also need to take insulin if other medications do not work well enough. There are different types of insulin available, such as rapid-acting, short-acting, intermediate-acting, and long-acting insulin.
• Metformin: This is an oral medication that lowers blood glucose levels by reducing liver glucose production and increasing muscle glucose uptake. Metformin is usually the first-line medication for people with type 2 diabetes who do not have kidney problems.
• Sulfonylureas: These are oral medications that lower blood glucose levels by stimulating pancreatic beta cells to release more insulin. Some examples are glipizide, glyburide, and glimepiride.
• Meglitinides: These are oral medications that lower blood glucose levels by stimulating pancreatic beta cells to release more insulin quickly after meals.Some examples are repaglinide and nateglinide.
• Thiazolidinediones: These are oral medications that lower blood glucose levels by increasing muscle and fat tissue sensitivity to insulin. Some examples are pioglitazone and rosiglitazone. Dipeptidyl peptidase-4 (DPP-4) inhibitors: These are oral medications that lower blood glucose levels by inhibiting an enzyme that breaks down incretin hormones, which stimulates insulin secretion and reduce glucagon secretion after meals. Some examples are sitagliptin, saxagliptin, linagliptin, and alogliptin. Glucagon-like peptide-1 (GLP-1) receptor agonists: These are injectable medications that lower blood glucose levels by mimicking incretin hormones, which stimulate insulin secretion and reduce glucagon secretion after meals. They also slow down gastric emptying and reduce appetite and food intake.