Ankylosing spondylitis is a type of arthritis that mainly affects the sacroiliac joints (where the spine meets the pelvis) and the vertebrae of the spine. Over time, chronic inflammation can lead to the fusion of spinal bones, causing the spine to become less flexible and, in severe cases, resulting in a forward-stooped posture.
AS is a form of seronegative spondyloarthritis, meaning it does not show rheumatoid factor in blood tests, which often distinguishes it from other types of arthritis like rheumatoid arthritis.
Who Is Affected?
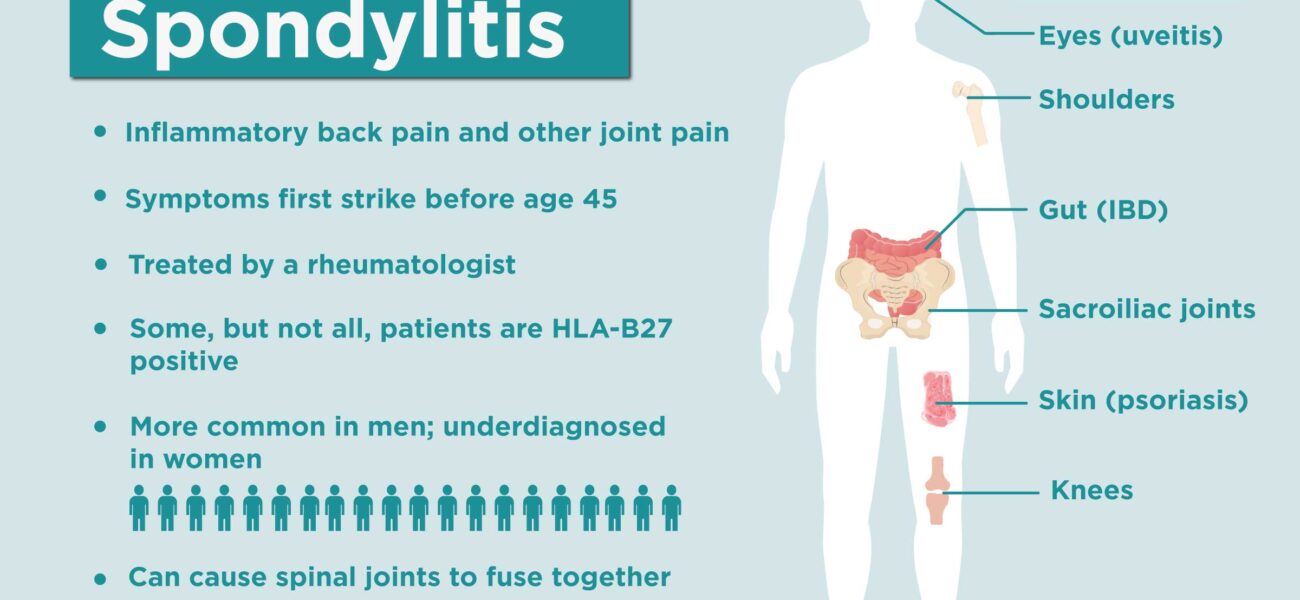
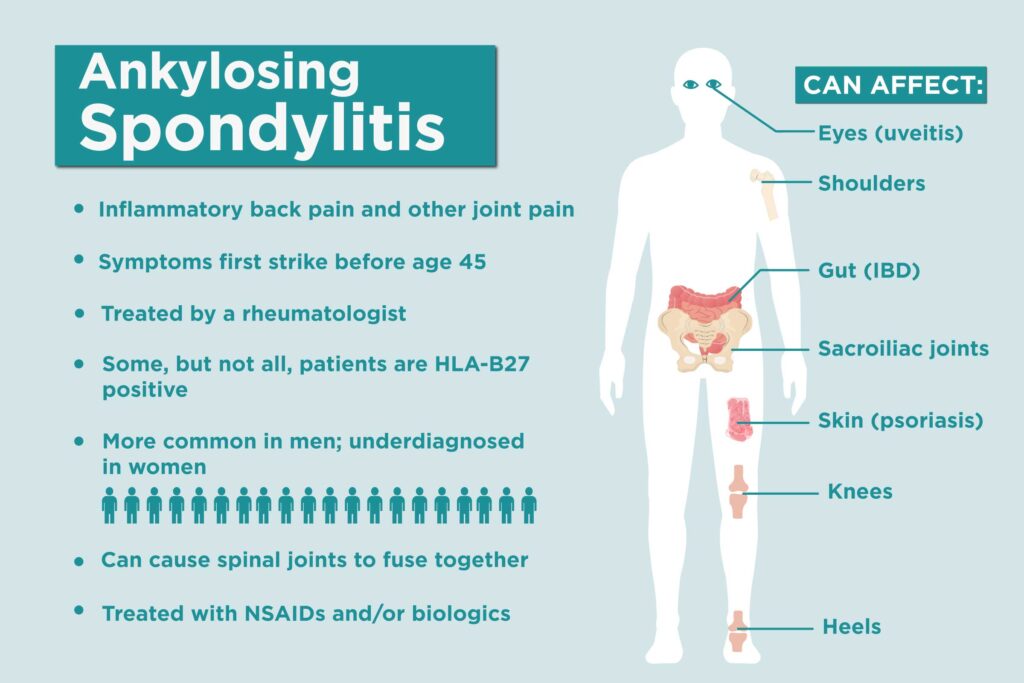
Ankylosing spondylitis typically begins in early adulthood, often between the ages of 17 and 35. It affects men more frequently than women, and genetics play a significant role. A specific gene called HLA-B27 is commonly associated with a higher risk of developing AS, though not everyone with the gene will get the disease.
Symptoms of Ankylosing Spondylitis
Symptoms usually develop gradually over months or years and can vary greatly between individuals. Common signs include:
- Chronic back pain and stiffness, particularly in the lower back and hips
- Pain that improves with exercise but not with rest
- Morning stiffness that lasts for more than 30 minutes
- Fatigue due to ongoing inflammation
- Reduced flexibility in the spine
- Pain in other joints, like the shoulders, knees, and heels
- Eye inflammation (uveitis), leading to redness, pain, and sensitivity to light
In more advanced stages, the spine may fuse, severely limiting movement.
Causes and Risk Factors
While the exact cause of AS is not fully understood, several factors appear to contribute:
- Genetic predisposition: Presence of the HLA-B27 gene greatly increases risk.
- Environmental triggers: Infections or other environmental factors may trigger the immune response leading to AS.
- Family history: Having a close family member with AS increases the likelihood of developing the disease.
How Ankylosing Spondylitis Is Diagnosed
Diagnosing AS can be challenging because early symptoms are often mistaken for mechanical back pain. To make an accurate diagnosis, doctors may use:
- Medical history and physical exam: Checking for signs like limited spinal movement and tenderness over sacroiliac joints.
- Imaging tests: X-rays or MRI scans can reveal early changes in the sacroiliac joints and spine.
- Blood tests: To check for markers of inflammation and the presence of HLA-B27.
Early diagnosis is crucial for slowing disease progression and preventing long-term damage.
Treatment Options for Ankylosing Spondylitis
There is no cure for AS, but treatments aim to reduce symptoms, maintain spinal flexibility, and prevent complications.
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are usually the first line of treatment.
- Disease-modifying antirheumatic drugs (DMARDs) may be used if peripheral joints are affected.
- Biologic agents, particularly TNF inhibitors and IL-17 inhibitors, have transformed AS management by targeting specific pathways in the inflammatory process.
- Physical therapy:
Regular exercise and stretching routines help maintain posture, flexibility, and strength. - Lifestyle modifications:
- Good posture practices
- Quitting smoking (which worsens spinal damage)
- Staying active despite discomfort
- Surgery:
In rare cases, surgery may be needed to replace joints or correct severe spinal deformities.
Living with Ankylosing Spondylitis
Managing AS is a lifelong journey. Success often involves a combination of medical treatment, physical activity, and supportive therapies. Many people with AS are able to lead full, active lives with proper care.
Here are some tips for daily management:
- Stay consistent with prescribed exercises and physical therapy.
- Monitor for signs of eye inflammation or heart problems, as AS can affect other organs.
- Build a strong support network, including healthcare providers, family, and patient groups.
- Prioritize mental health, as chronic illnesses can sometimes contribute to anxiety or depression.
Final Thoughts
Ankylosing spondylitis may start silently, but its impact can be profound if left unchecked. Early recognition, proper treatment, and an active lifestyle are key to minimizing the effects of this chronic condition. With growing research and advancements in therapy, individuals with AS have more tools than ever to manage their health and maintain their independence.
If you or someone you know is experiencing persistent back pain, especially if it improves with activity, it’s important to consult a healthcare provider. Early intervention can make a world of difference.
The list of some Ankylosing Spondylitis medicine:
ENDOL