Fusariosis is an infection caused by the Fusarium fungi, which can affect various parts of the body, including the skin, eyes, sinuses, lungs, and even internal organs like the liver and kidneys. The infection is most commonly seen in immunocompromised individuals, though it can also occur in individuals with chronic diseases such as diabetes.
Fusariosis typically develops when Fusarium spores, which are found in the environment, enter the body through a break in the skin or are inhaled into the lungs. Once inside the body, these fungi can cause a range of symptoms, from mild to severe, depending on the area affected and the health of the individual.
Causes and Risk Factors
Fusariosis is caused by various species of the Fusarium fungus, with Fusarium solani and Fusarium oxysporum being the most common culprits. These fungi can infect humans in several ways:
- Inhalation of spores: Individuals with compromised lung function or weakened immune systems may inhale Fusarium spores from the environment, leading to respiratory infections.
- Breaks in the skin: Fungal spores can also enter through cuts, abrasions, or other breaks in the skin, causing localized infections.
- Invasive medical procedures: Procedures like organ transplants, the use of catheters, or prolonged antibiotic therapy can increase the risk of Fusarium infection by disrupting normal body defenses and allowing the fungus to invade.
Key Risk Factors for Fusariosis Include:
- Immunocompromised states: Patients with conditions such as leukemia, lymphoma, HIV/AIDS, and those undergoing chemotherapy or organ transplantation are more susceptible.
- Prolonged use of corticosteroids: These drugs suppress the immune system and can increase the risk of fungal infections like fusariosis.
- Chronic diseases: Diabetes, especially when poorly controlled, can weaken the body’s ability to fight off infections.
- Trauma or burns: Open wounds or burns provide an entry point for the fungi to invade the body.
The risk of developing fusariosis is highest in individuals who have a weakened immune system, as their body’s defenses are less capable of combating the infection.
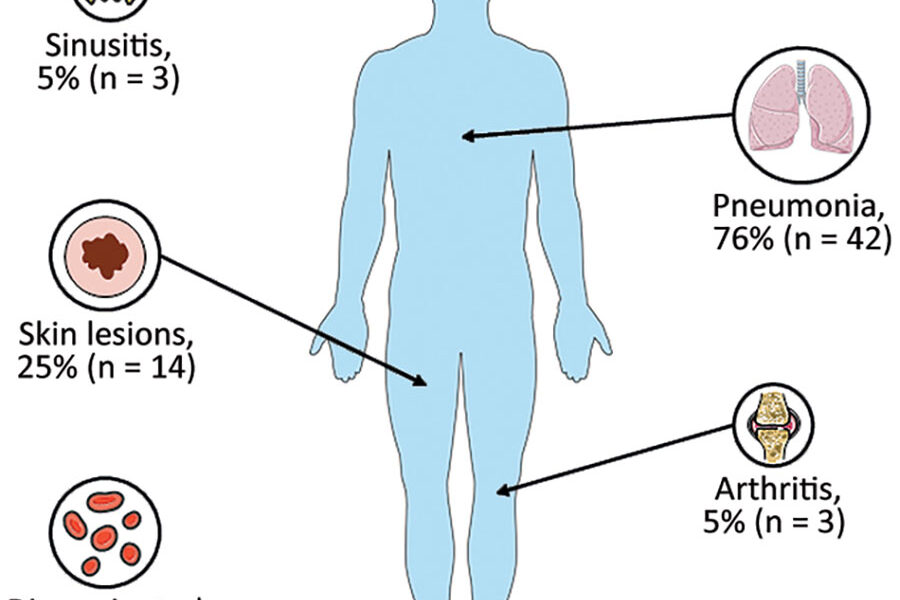
Symptoms of Fusariosis
The symptoms of fusariosis can vary widely depending on the area of the body affected. Common symptoms include:
Skin Infections:
- Red, swollen, painful lesions: These may appear as small bumps or nodules, sometimes with a necrotic (dead tissue) center.
- Ulcers or abscesses: In some cases, the infection can lead to open wounds or pus-filled abscesses.
Respiratory Infections:
- Fever and cough: Persistent fever, along with a dry cough, is common in pulmonary fusariosis.
- Chest pain: As the infection progresses in the lungs, it can cause chest discomfort or pain.
- Shortness of breath: In severe cases, the infection can impair lung function, leading to difficulty breathing.
Systemic Infections:
- Fever and malaise: Fusariosis can affect internal organs, leading to systemic symptoms such as fever, fatigue, and general discomfort.
- Organ failure: In advanced cases, the infection can spread to organs like the liver, kidneys, or heart, potentially leading to organ failure.
In severe cases, fusariosis can progress rapidly, particularly in immunocompromised individuals, and can lead to serious complications, including septic shock and death.
Diagnosis of Fusariosis
Diagnosing fusariosis requires a combination of clinical evaluation, imaging studies, and laboratory tests. Because the symptoms of fusariosis can overlap with those of other infections, it can be challenging to diagnose.
Diagnostic Tools Include:
- Clinical evaluation: A doctor will assess symptoms, risk factors, and medical history, especially any underlying immune system conditions.
- Microbiological cultures: Samples of infected tissue, blood, or sputum are collected and cultured to identify the presence of Fusarium fungi. This can help confirm the diagnosis.
- Imaging studies: Chest X-rays or CT scans may be used to identify fungal growth in the lungs or other internal organs.
- Histopathological examination: A biopsy of infected tissue may be taken to examine under a microscope for fungal elements, confirming the presence of Fusarium species.
Early and accurate diagnosis is crucial, as the infection can rapidly spread and cause significant damage to the body, especially in individuals with compromised immune systems.
Treatment of Fusariosis
Fusariosis is a serious infection that requires prompt treatment. The treatment approach depends on the severity of the infection and the health of the patient. The primary treatment for fusariosis involves antifungal medications, and the therapy must be tailored to the individual’s specific condition.
Antifungal Medications:
- Voriconazole: This is often the first-line treatment for invasive fusariosis, as it has been shown to be effective against Fusarium species.
- Amphotericin B: In severe cases, amphotericin B, a powerful antifungal drug, may be used intravenously.
- Posaconazole and Isavuconazole: These antifungal drugs are also options for treating fusariosis, particularly for patients who cannot tolerate voriconazole.
Surgical Intervention:
In cases where the infection has caused significant tissue damage, such as in skin infections or abscesses, surgical removal of infected tissue may be necessary.
Supportive Care:
Supportive care, including oxygen therapy for respiratory involvement or intensive care for severe infections, may be required in some cases. This can help manage symptoms and improve outcomes while the antifungal medications work.
Prevention of Fusariosis
Preventing fusariosis primarily involves reducing exposure to Fusarium spores and managing risk factors, especially in immunocompromised individuals. Some preventive measures include:
- Environmental controls: Hospitals and healthcare settings can use air filtration systems to reduce fungal spores in the environment. Immunocompromised patients may also be placed in specially designed rooms to limit fungal exposure.
- Protective measures: People at high risk should avoid exposure to soil, decaying plant material, or areas where mold is prevalent. Protective gloves and masks can help reduce the risk of infection.
- Prophylactic antifungal therapy: For high-risk patients, such as those undergoing chemotherapy or organ transplantation, antifungal medications may be given as a preventive measure.
Final Thoughts
Fusariosis is a serious and often life-threatening fungal infection that primarily affects those with weakened immune systems. Its symptoms can be diverse, and early detection and treatment are essential for improving the chances of recovery. With the right medical care, including antifungal medications and, in some cases, surgical intervention, individuals with fusariosis can successfully recover. If you or someone you know is at increased risk for fusariosis, it’s crucial to stay vigilant for signs of infection and seek medical attention promptly if symptoms occur. Awareness, prevention, and early treatment are the keys to managing this challenging fungal infection.
The list of some Fusariosis medicine: