Kidney transplantation offers a new lease on life for individuals with end-stage renal disease. However, despite advancements in surgical techniques and immunosuppressive therapies, acute renal graft rejection remains one of the major hurdles following a transplant. Recognizing, managing, and preventing rejection are key to ensuring long-term success of the transplanted kidney.
In this blog, we’ll dive into what acute renal graft rejection is, why it happens, how it can be detected early, and the strategies used to combat it.
Acute renal graft rejection occurs when the body’s immune system recognizes the transplanted kidney as foreign and attacks it. This usually happens within the first few months after transplantation but can also occur later.
Unlike chronic rejection, which progresses slowly over time, acute rejection tends to develop quickly and can lead to rapid loss of kidney function if not treated promptly. Thanks to modern immunosuppressive medications, the incidence of acute rejection has significantly decreased, but it still poses a risk that requires vigilant monitoring.
Types of Acute Rejection
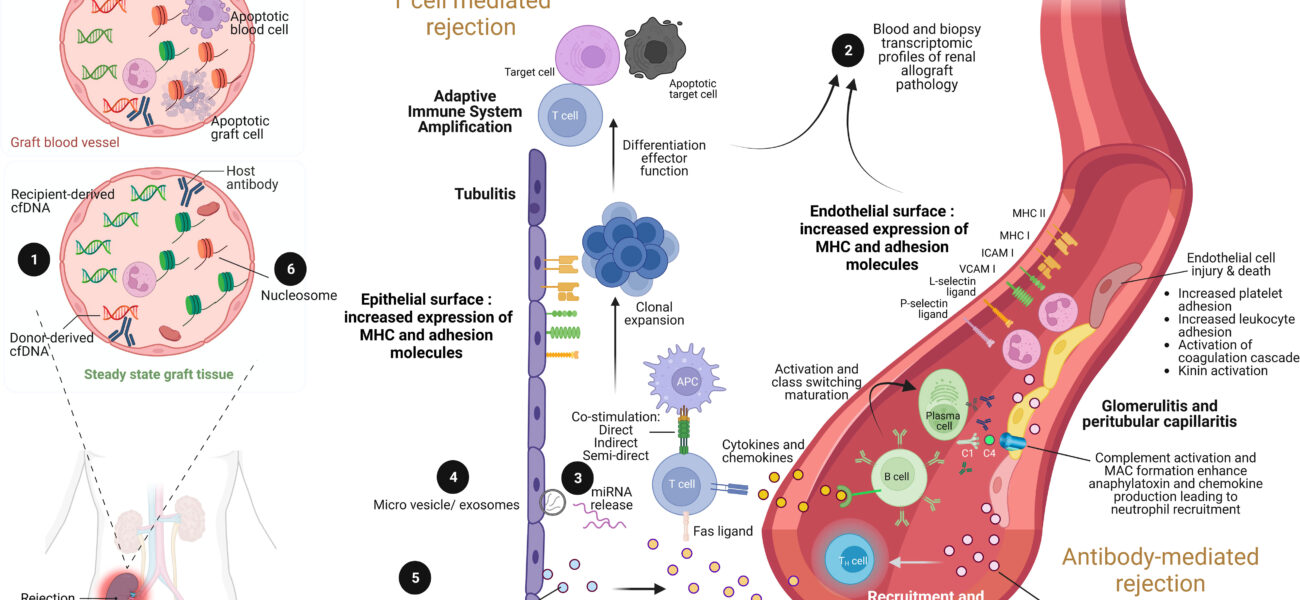
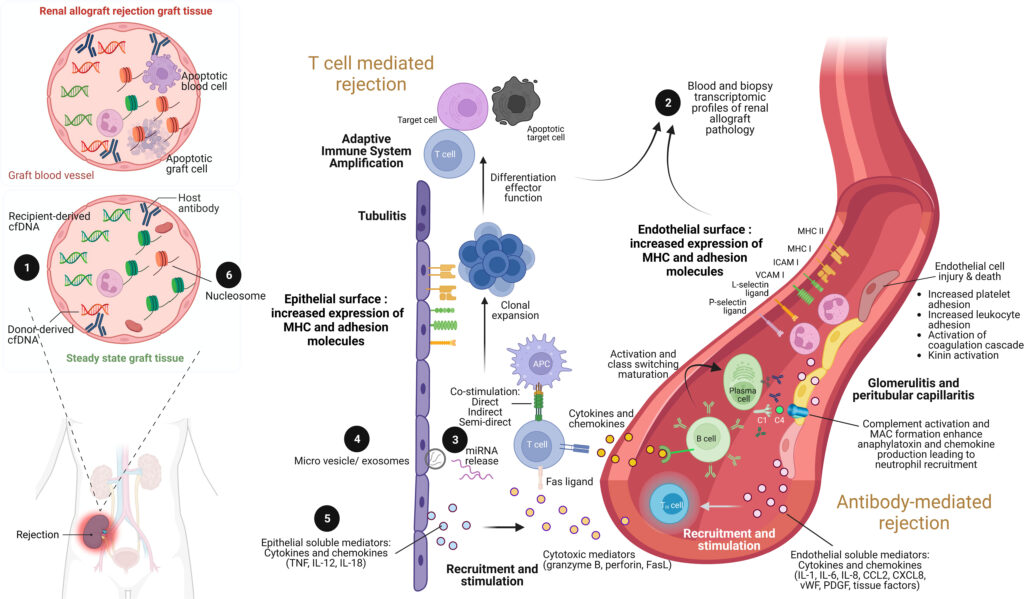
Acute renal graft rejection is generally classified into two types:
- Cellular (T-cell mediated) rejection: This is the most common form, where the body’s T-cells directly attack the kidney tissue.
- Antibody-mediated (humoral) rejection: Here, the body produces antibodies against the donor kidney, leading to inflammation and injury of the blood vessels within the graft.
Each type requires a specific approach to diagnosis and treatment.
Causes and Risk Factors
Several factors can contribute to the development of acute renal graft rejection, including:
- Nonadherence to immunosuppressive therapy: Skipping or stopping medications is a major trigger.
- HLA mismatch: Differences between the donor and recipient human leukocyte antigens (HLA) can increase the risk.
- Infections: Certain infections can stimulate the immune system and precipitate rejection.
- Inadequate immunosuppression: Under-dosing or poor absorption of medications can leave the graft vulnerable.
- Sensitization: Prior transplants, blood transfusions, or pregnancies can cause the recipient to develop antibodies against donor tissues.
Understanding and managing these risks is crucial to protecting the transplanted kidney.
Signs and Symptoms
Acute rejection can sometimes be “silent,” showing few symptoms early on. However, when signs do appear, they may include:
- Decreased urine output
- Swelling, especially in the legs or ankles
- Weight gain from fluid retention
- High blood pressure
- Fever
- Pain or tenderness over the transplant site
- Rising levels of creatinine in blood tests (an important marker of kidney function)
Regular follow-up and blood tests are essential to catch signs of rejection early.
Diagnosis
Prompt and accurate diagnosis is critical for effective treatment. Diagnostic steps typically include:
- Blood tests: Monitoring creatinine levels and other kidney function markers.
- Ultrasound imaging: Checking for swelling or blood flow issues in the transplanted kidney.
- Biopsy: The definitive method for diagnosing acute rejection involves taking a small sample of kidney tissue for microscopic examination. This helps differentiate between cellular and antibody-mediated rejection and guides treatment decisions.
Treatment Options
Acute renal graft rejection is a medical emergency that requires immediate intervention. Treatment typically involves:
- High-dose corticosteroids: The first line of treatment for cellular rejection.
- Anti-thymocyte globulin (ATG): Used in more severe or steroid-resistant cases.
- Plasmapheresis and intravenous immunoglobulin (IVIG): Commonly employed to remove harmful antibodies in antibody-mediated rejection.
- Rituximab or other targeted therapies: In some cases, medications targeting specific immune cells may be used.
The goal of treatment is to halt the immune attack, restore kidney function, and preserve the transplanted organ.
Preventing Acute Renal Graft Rejection
While not all cases of rejection can be prevented, several measures can significantly reduce the risk:
- Strict adherence to immunosuppressive therapy: Taking medications exactly as prescribed is the cornerstone of prevention.
- Regular monitoring: Frequent blood tests and check-ups help detect problems early.
- Prompt treatment of infections: Keeping infections under control helps minimize immune system activation.
- Healthy lifestyle: Maintaining a balanced diet, avoiding smoking, and managing conditions like diabetes and hypertension support overall graft health.
Education and counseling of transplant recipients play a crucial role in reinforcing these preventive strategies.
Final Thoughts
Acute renal graft rejection, although serious, is not an inevitable outcome for kidney transplant recipients. Early recognition, aggressive treatment, and diligent prevention strategies have dramatically improved the prognosis for those facing rejection.
A successful transplant journey is a partnership between patients and healthcare providers, built on communication, vigilance, and commitment to ongoing care. With modern medical advancements and patient empowerment, many kidney transplant recipients enjoy years—often decades—of excellent graft function and a significantly improved quality of life.
If you or a loved one has undergone a kidney transplant, remember: staying informed and proactive is one of the best defenses against acute rejection.
The list of some Acute Renal Graft Rejection medicine:
Myfortic